State Medicaid Managed Care Reforms: Delivering for Taxpayers, Patients, and Community Pharmacies
While the fight against Pharmacy Benefit Manager (PBM) abuse continues at the federal level, states have been stepping up to steadily implement PBM reforms within a critical area of prescription benefits… Medicaid.
West Virginia’s Pioneering Move
In 2016, West Virginia took the lead by “carving out” prescription benefits from Medicaid Managed Care (MMC) programs. They shifted these benefits back to the fee-for-service program after realizing that promised savings from Medicaid Managed Care Organizations (MCOs) and their PBMs did not materialize. The result? West Virginia achieved $54.5 million in savings while ensuring that pharmacies received $116 million more to cover claims costs. Ohio followed suit, exposing MCO PBM overbilling to the tune of $288 million. This led to a four-year reform effort, closely supported by IPC’s Government Relations Department and the Ohio Pharmacists Association. The reform mandated cost-based pass-through reimbursement for MMC Rx claims based on NADAC (National Average Drug Acquisition Cost) and a professional dispensing fee tied to Medicaid’s Cost of Dispensing (COD) survey.
National Leadership and the Benefits for Community Pharmacy
IPC’s Government Relations Department has continued to lead nationally, collaborating with industry partners in four other states (CA, FL, MI, NY). These states are enacting either Medicaid Rx “carve outs” or MMC Rx reforms similar to those achieved in Ohio’s. The key benefits for independent pharmacies include:
Full Reimbursement for Drug Costs:
- Reimbursement is based on NADAC, WAC (Wholesale Acquisition Cost), or state-maintained MACs (Maximum Allowable Costs) for generics.
- Transparency ensures appeal rights to the state; not the PBM, for below acquisition cost prices.
Professional Dispensing Fee (PDF):
- Determined by the state based on the Medicaid Cost of Dispensing (COD) survey.
- No longer subject to the PBM’s arbitrary fee (typically $0.25-$0.75).
Final Payment at Cost Basis:
- Unless there’s a fraud accusation by the PBM, no more post-claim clawbacks.
- Ensures fair compensation for pharmacies.
Expanded Drug Availability:
- Legislation helps to preserve full Medicaid Managed Care patient care access to pharmacy services from the community pharmacy of their choice.
- Pharmacies can feel comfortable carrying the drugs they need for their vulnerable Medicaid patients without the worry of financial constraints.
Comprehensive Services:
- Full cost-based reimbursement allows pharmacies to provide essential services to patients with multiple disease states.
Real Savings and Continued Advocacy
These transparent, cost-based Medicaid Managed Care prescription drug reimbursement programs (in KY, MI, OH) and full carve-outs back to fee-for-service (in CA, ND, NY, WV) have resulted in significant policy outcomes. States have saved nearly a billion dollars by ending Medicaid overpayments to MCO PBMs. These savings complement the eighteen state Medicaid fraud settlements against Centene, totaling nearly $1 billion in recovered funds.
States with Medicaid Managed Care Prescription Benefit Reform Initiatives 2024:
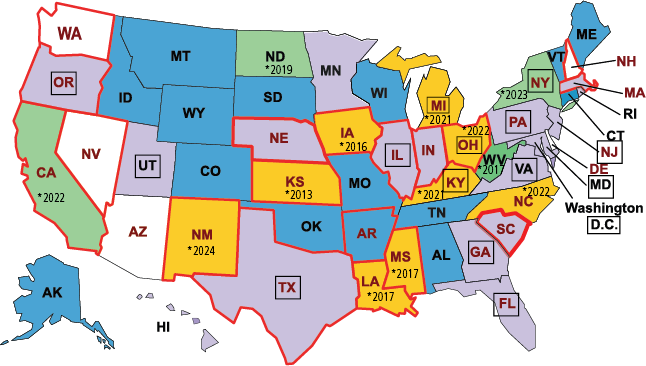
As more states consider MCO Rx reforms, IPC’s Government Relations team remains committed to leading reform efforts. Our expertise and experience will continue to drive positive change through state legislation or regulatory actions to enhance Medicaid managed care.
What can you and your pharmacy do to help?
As a pharmacy, you play a crucial role in shaping policy and advocating for positive change. Here are actionable steps you can take to make a difference:
Engage with Legislators:
- When advocacy campaigns are underway, we actively respond to messages from professional organizations, advocacy groups, and legislative offices. Your voice matters, and your input can influence decisions.
- Visit the IPC Legislative Action Center: Regularly check your state or national pharmacy association’s website for updates. Participate in campaigns, sign petitions, and share your perspective on critical issues affecting pharmacies and patients.
- Extend invitations to your local legislators to visit your pharmacy. Show them firsthand the impact of policies on your daily operations, patient care, and community well-being.
Provide Personal Testimony:
- Legislators need to hear real stories from pharmacists. Prepare concise and compelling testimonies about challenges you face, patient interactions, and the importance of fair reimbursement.
- Emphasize how your pharmacy contributes to patient health, especially for vulnerable populations. Describe the services you provide beyond dispensing medications.
Educate and Collaborate:
- Host informational sessions or workshops for patients, community members, and other healthcare professionals. Explain the intricacies of pharmacy reimbursement and the impact of policy decisions.
- Join forces with other local pharmacies, healthcare providers, and patient advocacy groups. Together, you can amplify your advocacy efforts.
Stay Informed:
- Keep up-to-date with legislative proposals, regulations, and industry trends. Understand how changes may affect your pharmacy’s viability and patient care.
- Participate in pharmacy association meetings, webinars, and conferences. Learn from experts and network with colleagues.
Use social and Traditional Media:
- Share advocacy messages, success stories, and relevant news on your pharmacy’s social media channels. Engage with followers and encourage them to join your cause.
- Submit opinion pieces to local newspapers or industry publications. Explain why specific policies matter and how they impact your community.
Remember, advocacy is a collective effort. By actively participating and advocating for fair policies, you contribute to a stronger pharmacy profession and better patient outcomes. Let your voice be heard!